© 2024 Generations Hospice
All Rights Reserved
All Rights Reserved
We don’t often think about the importance of staying hydrated. We may go for hours and hours without a sip. We may wait until we’re thirsty to get a drink.
Generally, you should drink ⅓ of your weight (in pounds) in ounces of water daily. For example, if you weigh 150 pounds, drink 50 ounces of water (or other hydrating beverages) daily.
Many health problems and medications can affect the amount of water we need, so it’s best to talk with your doctor about your specific needs.

As we get older, our ability to regulate the amount of water in our body declines. What’s more, our lifestyle and habits may change over time. We may have been more active, naturally drinking more water. But now we don’t exercise as much or at high intensity.
We may have commuted to work every day with a drink in the cup holder. We sat at our desks with a tumbler of water within reach, a constant reminder to take a drink.
For seniors, we need to maintain a 55% level of water in our bodies. Dehydration, even in mild cases, can harm health and exacerbate existing medical conditions. Symptoms like confusion, dizziness, fatigue, joint pain and constipation can result from inadequate hydration.
The importance of staying hydrated extends beyond everyday life for seniors. It becomes even more critical when recovering from an illness, injury, or medical procedure. During these times, the body requires additional support to heal and regain strength and adequate hydration plays a vital role.
Some of the ways hydration helps you heal include:

Many of us take multiple medications, some of which may cause an increase in urination. What’s more, many chronic health conditions, like diabetes and kidney disease, can contribute to this loss of fluids. Losing too much fluid is even more dangerous in summer.
During the hotter months, the combination of higher temperatures and perspiration can lead to a greater risk of dehydration. Heat-related illnesses like heat exhaustion and heat stroke are also more common in seniors and can be life-threatening.
Look for shade, go into an air-conditioned building, and avoid prolonged exposure to heat and sun when temperatures and humidity rise.
Drinking enough water isn’t the only way to prevent dehydration. Other hydrating beverages and foods are also options.
Foods like fruits and vegetables with high water content can help also us stay hydrated: strawberries, tomatoes, watermelon, celery, and cucumbers. Beverages like herbal teas can increase hydration too. But it’s essential to limit caffeine and alcohol. They can have a diuretic effect.
Remember that staying hydrated is important at any age but is critical for seniors. Staying hydrated gives our bodies the necessary support to heal, manage medications, boost immune function and regain energy and mobility. Be sure to talk with your doctor about their hydration recommendations for your needs.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2908954/
https://www.ncoa.org/article/how-to-stay-hydrated-for-better-health
Watching someone you love suffer from Alzheimer’s or another memory debilitating illness is incredibly difficult, and it can be even more challenging to decide when it’s time to consider hospice care. Here, we are sharing five signs it may be the right time to consider the extra support of hospice care for an Alzheimer’s patient.
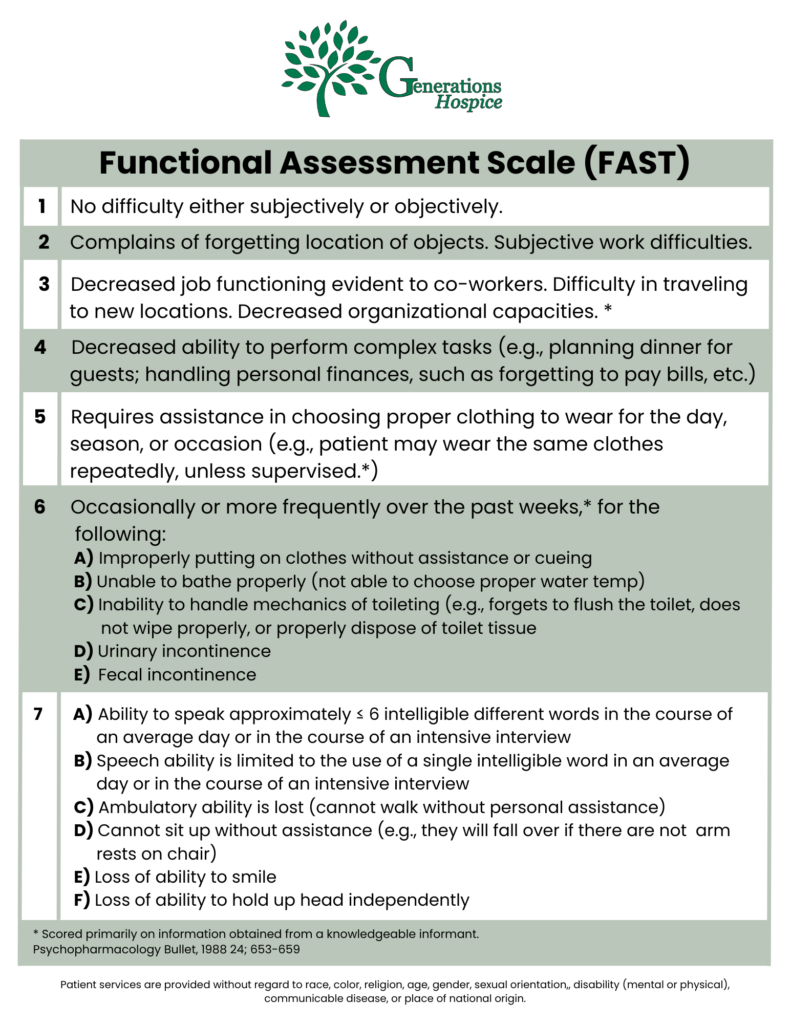
The Functional Assessment Staging (FAST) Scale is a tool used to determine if changes in a patient’s condition are related to Alzheimer’s disease or another condition. If due to Alzheimer’s, the changes will occur in sequential order. Alzheimer’s disease-related changes do not skip FAST stages.
This means a person is no longer able to get around on their own. For example, they require assistance getting from room to room.
Without assistance, you may notice they put their shoes on the wrong feet or their day-time ‘street’ clothes on over their pajamas. They are also unable to bathe without assistance.
This includes urinary or fecal incontinence or both.
This may begin as the patient only saying 5-6 words per day and gradually reduce to only speaking one word clearly until they can no longer speak or communicate at all. This will also include the inability to smile.

Hospice care is for patients with a life limiting illness and a life expectancy of six months or less. The main focus is to manage pain and symptoms and ultimately keep the patient comfortable. When you choose hospice for your loved one, their care team can help you to understand what to expect in the final stages of Alzheimer’s. They will also provide support to you and the rest of your family throughout the end-of-life process.
If you would like more information on hospice care for Alzheimer’s patients, please contact us. We are here to answer any questions you may have.
Some older adults and people with serious illnesses, unfortunately, experience the end of life in certain healthcare settings that do not align with their desired wishes. If you have a serious illness or are a caregiver of someone planning end-of-life care, knowing the difference between palliative care and hospice care can help you make an informed decision when the time comes to transition to one of these healthcare settings.
Palliative care is a form of care that focuses on improving your quality of life and that of your family when you are living with a serious illness. It focuses on your whole-person health rather than only on your condition. If you are receiving palliative care, your treatment plan may focus on reducing symptoms of your illness and on improving secondary conditions such as depression, sleep deprivation, and side effects of medications.
Palliative care may be given in various healthcare settings, such as at the hospital, a residential care facility, or your home. Anyone can receive this type of care regardless of age or the severity of their condition.
If you receive palliative care, you may work with and be treated by various healthcare professionals, including doctors, nurses, social workers, pharmacists, physical therapists, counselors, and nutritionists. If you need spiritual care, your palliative care team may even include a chaplain. The healthcare professionals that make up your palliative care team will depend mainly on your recovery needs and level of care.
Studies show that palliative care offers many benefits, including:

Hospice care focuses on improving your comfort and quality of life when you are nearing the end of your life. This type of care is usually given in circumstances in which an illness continues to progress despite treatment or when the patient chooses not to receive certain treatments. Hospice care is similar to palliative care in that it provides comfort care and support for the family. However, treatments are not given to improve the illness.
Like palliative care, hospice care can be given in many different healthcare settings, though it is most frequently given at your home, where you can be most comfortable and spend quality time with your loved ones. In addition, it is typically given when your healthcare provider believes you have no more than six months to live. Some benefits of hospice care include 24/7 access to nurses and healthcare workers who can address and relieve symptoms and side effects and access to medical equipment and medications that can reduce your discomfort.
Many of the same types of healthcare professionals that make up a palliative care team will also be part of your hospice care team. This includes doctors, nurses, social workers, chaplains, and volunteers who dedicate their time to giving you the support you need and making you feel as comfortable as possible during your final months.
To be eligible for hospice care, you will discontinue aggressive treatment efforts to combat your terminal illness (such as experimental surgeries, aggressive chemotherapy, or other treatments that require prolonged hospitalization and recovery). However, you may continue to receive treatments for other conditions, such as antidepressants to treat depression or insulin medicines to control Diabetes.
Comfort care and end-of-life care are both terms that describe the type of care you receive when you are near the end of your life and are no longer receiving treatment for your illness. It is highly similar to palliative care in providing you with whole-person care that focuses on your physical, social, emotional, and spiritual health. Comfort care and end-of-life care may include palliative care or hospice care, or a combination of both.
Sometimes, palliative care is given as part of hospice care, and both types share many similarities. For instance, the goal of both palliative and hospice care is to improve your quality of life and help you find relief from painful and severe symptoms and side effects of treatment. Both types of care also focus on whole-person health. However, there remain many differences between palliative care and hospice care.
Some of these differences are:

You may want to consider palliative care if you or your loved one has a serious illness or chronic condition that requires long, intensive care or that causes severe physical symptoms and/or emotional distress. For example, cancer, heart disease, AIDS, and kidney failure are some of the many conditions that can benefit from palliative care.
Additionally, palliative care may benefit you if you:
A person may transition from palliative care to hospice care if their doctor thinks they have no longer than six months to live. Sometimes, it can be difficult for doctors to predict exactly how long it will take for a particular disease to run its course or how long a person has left to live if their health is in decline. In these circumstances, it’s important to consider how transitioning to hospice care could improve your quality of life during your final months.
According to the National Library of Medicine (NLM), doctors should strongly consider referring chronically ill patients to hospice care if they spend more than half their time in bed, are unable to function efficiently, and are experiencing both physical and psychological distress. The NLM adds that hospice referrals are usually necessary when the patient’s condition has progressively declined to the point that their highest priority is to take control of their healthcare and achieve the greatest possible comfort in their homes as they near the end of life.
Talk to your doctor if you think you may need hospice care but aren’t sure when you should transition out of palliative care. Your doctor can talk to you at length about your options and the benefits of transitioning to hospice care based on your condition and unique circumstances.
Taking advantage of hospice care as soon as it’s needed could result in access to quality care and lots of extra quality time to spend with your loved ones. Additionally, studies show that patients who plan their care in advance are more likely to be satisfied with their care, given how they can make decisions that align with their end-of-life wishes.
Consult with your healthcare provider if you or your loved one is interested in learning more about palliative care or hospice care. Your doctor can refer you to a palliative or hospice care specialist who can answer all your questions and help you determine which of these services may be more ideal.
Palliative care and hospice care are covered by many major health insurance providers, including Medicare. The exact benefits covered will vary based on your health plan. Benefits covered may include medical equipment and supplies, skilled nursing care, bereavement support, and medications to provide comfort, among many others.
Hospice At Your Side has resources for home health and hospice services throughout the United States. Specialty services we offer include diabetes care, orthopedics, and pain management. Call us today to learn more about our many home healthcare services.

We all grieve differently, but one thing remains true for everyone: the importance of taking care of yourself. Whether you’ve found yourself in a state of just going through the motions or you’ve put all your focus on taking care of your loved ones, it can be easy to put your own needs on the back burner when facing the loss of a loved one.
However, it’s absolutely imperative that you take time to focus on yourself, too. In honor of Mental Health Awareness Month, we are discussing the importance of self-care throughout the grieving process.
Mental Health Awareness Month dates all the way back to 1949 when the National Association for Mental Health (now known as Mental Health America) first organized the observance in the month of May to help raise awareness and lessen the stigma attached to mental illness.
For a long time, society looked at mental illness as being just one thing. There was always a negative stigma attached to the term, and people often thought of those living with a mental illness as having ‘gone mad’. However, that is simply not true. Over time, we’ve learned more about the many layers and types of mental illness.
Mental illness is the term used to describe mental health conditions that impact a person’s mood, thinking, and behavior. Common mental illnesses include:
Losing a loved one can be a traumatic experience. You may feel as though you lost a part of yourself and that your life will never be the same. While there is some truth to this, it’s important to remember that you are still here and must go on living your life.
“We don’t move on from grief. We move forward with it.”
Feelings of sadness, anger, loneliness, and hopelessness are all common throughout the grieving process. However, these feelings can sometimes develop into chronic grief which can in turn become a mental illness. In some cases, grief can lead to depression.
Symptoms of chronic grief can include:
Self-care used to be thought of as bubble baths and pampering yourself, but there is much more to self-care. Just like the grieving process, self-care can look different for everyone. But the overall concept is to take care of yourself physically, mentally, and emotionally.
To take care of yourself physically is pretty simple: eat a well-balanced diet, drink plenty of water, exercise regularly, and practice healthy hygiene habits. However, taking care of yourself mentally is a little less cut and dry. This is where it really differs from person to person. To take care of yourself mentally and emotionally, you need to take time to do the things that make you feel good and happy. Hobbies are a good place to start when focusing on taking care of yourself mentally. Maybe you enjoy sitting outside and reading a good book, maybe you are an artist, maybe you enjoy taking long walks with your dog. Whatever it is that leaves you feeling happy and fulfilled, do it!
Research shows the more you practice self-care, the more confident, creative, and productive you are. This also leads to experiencing more joy, making better decisions, building stronger relationships, and communicating more effectively. Overall, you will be in a better frame of mind, making you a better version of yourself. This is not only good for you, but it’s also good for those who depend on you.
When you take time to take care of your whole self (physically, mentally, and emotionally), it will help you to process your feelings of grief in a healthier way.
Always remember that you do not have to face the journey of grief alone. Lean on friends and family to help you through. Don’t be afraid to talk about your feelings. Sometimes we feel the need to be strong for those around us. If this is the case and you would feel more comfortable talking to someone outside the family, lean on the support of your hospice bereavement team. Our kind, compassionate bereavement coordinators are always available to talk or just listen. Never hesitate to reach out.
If you or someone you love is struggling with their feelings of grief and would like to talk to one of our bereavement coordinators, please contact us at 920-922-0134.